It was my first emergency room visit just weeks after a double mastectomy direct-to-implant, when I realized that my intuition would be the very thing that saved my life. Angry that I was even in this position to begin with, I was especially irritated by the fact that I had to repeat myself eight times for the eight interns that visited, and all asked the stock questions.
I am an anomaly. I do not fall in line with the classic statistics or symptoms as a patient. Sitting in front of these strangers proved that point over and over. “No, I don’t get fevers when I’m sick or have an infection…ever,” I repeated. Still pretty fresh from surgery with nerve damage, I had very little feeling in my chest, especially at the incision site which now resembled more of a transition to becoming a zombie than a woman trying to save herself from the effects of a BRCA1 mutation. Because of that, pain was a non-issue.
After sitting in the ER for four hours, retelling my case to eight interns, and never receiving the consult with a plastic surgeon I requested, I had the gut feeling I was in for a long haul. My plastic surgeon was out of town at a conference, and it turns out, he was at the same conference as the plastic surgeon from this hospital. There was no qualified provider left as my back-up in case of emergency…the very emergency I was living. So, I was discharged with the wrong antibiotic because no tests were run, no cultures were taken, and no blood was drawn. And heck, I didn’t have a fever, so there was that. That visit would set the tone for what was about to unravel over the next several months.
A week passed and my surgeon was still MIA, so I visited my PCP concerned that I was literally coming apart at the seams. Again, not seeming too concerned, because after all, I had no fever, nausea or vomiting, the PA decided to swab some samples after my continued prompting, even though she really was not concerned. Four days later, my intuition proved right – I had an infection. Even more so, the antibiotic from the ER was not the right one to fight it because it was discovered that I had Pseudomonas, an antibiotic-resistant bacterium that I contracted from unsterile conditions in the hospital. It literally said that in my chart.
Imagine if my PA had not done the necessary swab? That kind of bacteria is the very kind that kills people. I followed the protocol religiously, and yet, the appearance of my breast was not improving. Rather than call my surgeon who was now back in town, my husband was adamant that we show up when his office opened first-thing in the morning, and demand to be seen. So, we did just that. My husband drove us 1.5 hours and we were first in line. Even after explaining what had transpired the weeks prior, my surgeon brushed me off, asking how I could be confident something was wrong. “Look for yourself.” And he did, with mouth wide open. No words, he feverishly took multiple samples and promptly inserted me in his surgical schedule the next day for implant removal, debriding of the wound, and new implants. My intuition had served me well once again.
The surgery went well, and my highly-regarded, award-winning surgeon did not feel I needed to be placed on antibiotics since I just finished a round for my Pseudomonas diagnosis. So, I was sent on my merry way. Again, the story replayed itself. My surgeon was out of town, no back-up provider to contact, and my incision was now becoming a hole in the side of my breast. No fever. No nausea. No vomiting. But I knew things weren’t right when I looked in that hole and saw black material. Multiple calls to the office nurse who then made multiple unanswered calls to surgeon. Calls to new plastic surgeons in the health system, calendars cleared, and another emergency surgery was in store for me. Turned out the Pseudomonas had never cleared the first time and was setting up camp in my chest cavity.
My health journey did not end after that implant removal and replacement. Today, after seven total surgeries on my chest, I am left with deformed and scarred breast tissue. Open wounds unhealed after implant removals left my new surgeon no choice but to close my chest with whatever was left. What began as an informed and highly researched decision to have BRCA1 surgery to help beat my odds of dying from cancer, nearly killed me because of poor care. It was my intuition and advocating for my health and my life that saved me.
So many women are raised to listen, be “good” and follow directions. Somewhere along the lines, many of these very women lose their voice. For some, that can be in their relationships, in their jobs, or in their journey to health and wellness. I am thankful that I was raised differently. Coming from a line of women with auto-immune diseases, and a long lineage of cancer survivors and those who have lost their battle with cancer, I learned very quickly that I must advocate for myself, or no one will. I took note early on that as women, we have the gift of intuition. We are connected to our bodies in a unique and sometimes mysterious way, that provides an insight unexplained by science and medicine.
I did all the right things before my BRCA1 surgery. I researched. I spoke with several physicians and surgeons. I consulted genetics counselors and leaned on friends who had undergone the same surgery. I chose and trusted a highly credentialed and highly regarded surgeon. In the end, none of that mattered. Not one ounce of that pre-surgery work is what saved my life. My voice, my trust in myself and my intuition saved my life. My need to be heard was far more vital to my well-being than my need to be seen as a compliant or “good” patient.
The greatest lesson learned from this continued journey to health? Women must serve as their own advocate. We must speak up for ourselves and not be easily disregarded by providers who think their credentials mean they are free from error. We must continue to be our biggest proponent, unwilling to be silenced when we know in our gut that something is wrong. We must remember that intuition is our greatest superpower.
About the author
Amy Neuman Proffitt is a proud wife, mother and stepmother to six, marketing professional, blogger, motivational speaker and BRCA1 previvor. She continues to share her knowledge and experience of her health journey to help other women feel empowered to own their health and wellness and become the best version of themselves. Amy created The HERo, a community of confident and empowered females who are their own HERo. This community continues to grow through in-person events and training for women of all ages, and online through social media platforms.

When I was diagnosed with the BRCA mutation in February of 2019, I knew I would have to get a double mastectomy. At that moment I could not pinpoint when a good time would be. Maybe after I get married? Maybe after I have children? Maybe when my kids are older? I was not ready to make that decision.
As months went by, I took measures to help myself physically and emotionally with the news. I got my annual MRI and made an appointment with an oncologist to discuss my options. I also decided to start training for the 2019 NYC marathon and raise money for Sharsheret- an amazing organization that helps women and their families face breast and ovarian cancer. The clear MRI was a huge relief, and running a marathon validated that I was healthy and in control of my diagnosis. However, I still needed to deal with the reality of my BRCA mutation.
My fiancé and I set up an appointment to go see my oncologist for the second time. There I decided that, in the summer of 2021, which would be months after our November 2020 wedding, I would have my double mastectomy. I felt better knowing that we had a set timeline that I would only have to do the intense surveillance for another year. Then we can move on with our lives!
However, 2020 had other plans. When COVID-19 first entered the United States, I really didn’t think it would affect our wedding date. It was March and our wedding was in November. This will certainly be done within 8 months! Yet as schools closed and large gatherings were being shut down, my fiancé’ and I realized that postponing our wedding would be the most realistic and safe option.
As much as it was a bummer that the wedding date was changing, I had something bigger on my mind. How was I going to get my double mastectomy in the summer of 2021 and then get married in November? Would I recover in time? What if I had complications? My entire timeline was turning upside down. I felt like I was losing control and my anxiety was through the roof.
Then, I had a crazy idea. Why don’t I just have my surgery this summer?
You may be thinking, “This woman is insane! We are in the middle of a pandemic! Why would you want to enter a hospital by choice?” Great question. I am a special education teacher at a public school in Manhattan. Having to take off work during the school year is a huge undertaking for a teacher. Organizing sub plans and coverage is more work than actually being there! Plus, I love my job. And now that our students are remote learning, I don’t want to miss a minute of in person teaching when we are back in the classroom. Summers, for me, are the only option.
Another question you may ask: “Why don’t you just wait until after the wedding to get your surgery?” Well, when you are diagnosed with the BRCA mutation, you are given a timeline. Breasts off by age X, have kids by age Y, ovaries out by age Z! Now that the wedding date has changed, I adjusted my timeline in the hopes that the rest of my plans go as anticipated. This enables me to feel more in control of my BRCA mutation, at least in some shape or form.
I describe having the BRCA mutation like this: Let’s say a bee lands on you. It may sting you, it may not. You could just leave it and wait until it starts to hurt. But wouldn’t you just rather get it off? That’s how I feel about getting my breasts removed. I totally understand that not everyone with the BRCA mutation feels this way. And that is ok! Please know that your reasoning is valid. We are all different and cope in various ways, and we should not judge one another based on the path we choose.
Now that our wedding has officially been changed to October 2021, the next step is to choose a surgeon and set a date. Finding a surgeon that is operating during a pandemic is not a walk in the park. Technically this is an elective surgery. Many oncologists are still operating, but not necessarily the plastic surgeons (who do the reconstruction after the oncologist performs the mastectomy). Currently I have two appointments lined up who have confirmed that they will operate. Crossing my fingers that we will set a surgery date for July! It sounds strange, but in a way I am looking forward to the summer surgery. I get to do something healthy for myself- that gives me an element of control of my future. At the end of the day, the decision keeps me safe.
I started this piece with a lot “maybe” questions about when I would have my double mastectomy. Though the timing of that decision has been made, there are still a ton of “maybes.”
Maybe I will get direct implants.
Maybe I will have them above the muscle, or maybe below!
Maybe I will choose to have a DIEP-Flap (where they take fat from other parts of your body and use it in your new breasts).
Maybe my fiancé and mom will be allowed to be with me in the hospital.
Maybe I will have to wear a mask the entire time I’m recovering.
Maybe I will have to get tested for COVID before I enter the hospital.
Maybe I will have to quarantine after the surgery.
A-lot of maybes. I never thought I would be getting my surgery at this time, let alone during a pandemic. Yet I know it’s the right decision for me, and for my timeline. I’ve been doing plenty of research, perhaps too much. I’ve had a few close calls when sharing screens with my students while teaching. The last thing I want them to see (instead of the math PowerPoint) is a video of a doctor taking out a woman’s drain tubes post-surgery! Because remote teaching isn’t ridiculous enough….
What’s the message of my story? “When we plan, God laughs.” Making these decisions is hard, but I prefer having maybes that represent options, then no options at all. I realize that the world keeps turning even when my plans seem solid and my timeline is defined. “Maybes” are tough, they give you a lot to think about. However, I appreciate having options and the opportunity to exert control of my BRCA mutation, and my life as well. I guess maybes aren’t so bad after all.

By Rachel Samuels
I remember very distinctly the day that I was tested for the BRCA 1 and 2 mutations. I sat patiently in my OBGYN’s office, staring at the posters about birth control… pregnancy… STDs, but none of them referencing the decision that I was about to make. I was choosing to be tested for a gene mutation that could increase my lifetime likelihood of breast cancer to 72% and ovarian cancer to 39%. But to be honest, I was pretty calm about the entire process. Why? Because I was all but certain that my results would come back positive.
By the time I was 16, I had lost by mother, grandmother and great aunt to breast cancer. This sad legacy was something that I was acutely aware of for most of my life. By the time I was born, my mother was already a 7 year breast cancer survivor. At age 27, she was diagnosed with a Stage 3 invasive ductal carcinoma in her right breast. She underwent a unilateral mastectomy all the way down to the chest wall. Despite several attempts, she was unable to reconstruct and lived my entire childhood with one breast. One of my earliest memories was looking up at her as she dressed, a ritual that always included the placement of a breast form. Twenty years ago, women didn’t have the same options that they do today. My mother’s prosthesis was a cumbersome, beige, silicone “breast” (a generous description) that required her to wear a “heavy duty” support bra at all times. If she wanted to wear a normal bra, she had an oval-shaped cotton pad that (roughly) mimicked the shape of a real breast. But she made do. At the end of the day, the most important thing was that she was alive… she was a survivor.
Just one month shy of my 14th birthday, while snooping through my mother’s mail, I discovered a wig catalog. I assumed that it was trash and as I went to throw it in the garbage, my mother stopped me — “We need to talk.” I don’t know how, but I knew in that instant that she had cancer again and that everything wasn’t going to be okay. It’s been 15 years since I lost my mom and I have tears in my eyes typing that last sentence. But that emotion is precisely why I am writing this blog today. My mother’s story wasn’t in vain. Because of that loss, I am strong, I am proactive — I am a previvor.
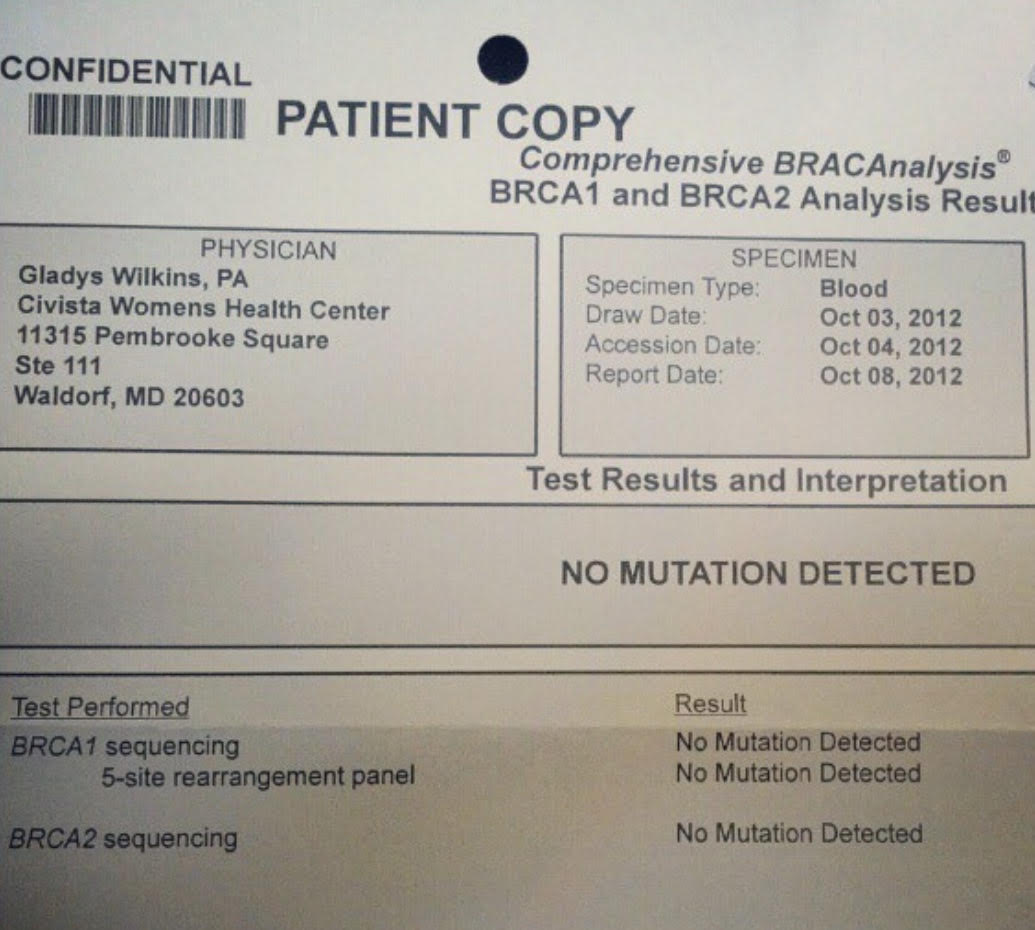
My journey to becoming a previvor started the day I was tested for BRCA. I was all but certain that this simple blood test was going to change the trajectory of my life. Flash forward one month. I walked to my mailbox and there it was – my genetic test results. With the wad of remaining mail tucked in my armpit, I ripped open the envelope and quickly scanned the page. NO MUTATION FOUND. I stopped and looked closer. NO MUTATION FOUND. I thought for certain that I was reading something wrong as I unlocked my front door. I sat down on the couch and read it again. NO MUTATION FOUND.
 I really wish I could have been a fly on the wall to capture my expression as I just stared at this single sheet of paper. For most women waiting for their results, there is a sense of anxiety… of waiting to hear if your life is going to change. As odd as it sounds, for me, it was almost worse finding out that I didn’t have BRCA. The same thought kept running through my head: What the heck is wrong with my family then? A BRCA mutation diagnosis is a starting point for many women. They assess their risk(s) and then decide on a course of action. But… I had already decided – a bilateral, prophylactic mastectomy. This would be an effort to prolong my life… a way to avoid the same sad fate as all of the women in my family. But what was I supposed to do now?
I really wish I could have been a fly on the wall to capture my expression as I just stared at this single sheet of paper. For most women waiting for their results, there is a sense of anxiety… of waiting to hear if your life is going to change. As odd as it sounds, for me, it was almost worse finding out that I didn’t have BRCA. The same thought kept running through my head: What the heck is wrong with my family then? A BRCA mutation diagnosis is a starting point for many women. They assess their risk(s) and then decide on a course of action. But… I had already decided – a bilateral, prophylactic mastectomy. This would be an effort to prolong my life… a way to avoid the same sad fate as all of the women in my family. But what was I supposed to do now?
I was incredibly fortunate to have a wonderful breast surgeon, Dr. Eleni Tousimis of Georgetown University Hospital. Dr. Tousimis listened to me as I voiced my concerns, reviewed my family history and together we mapped a plan of action. We would move forward with a preventative mastectomy. Dr. Tousimis reminded me that only 10% of women diagnosed with breast cancer have a BRCA 1 or 2 mutation, and that even though I had not tested positive for THESE gene mutations, it was possible that I might have another. Or even more likely, based on my family history, I may have a gene mutation that modern science simply hasn’t discovered yet.
I remember feeling very calm walking out of that appointment, which is odd considering the circumstances: I was a 25 year old woman who had decided to prophylactically remove both of my breasts to hopefully avoid the disease that had plagued my family. But you know what… the most important thing that I’ve learned on this journey is that the scariest part of it all is the fear of the unknown. This is why it is SO important that we get informed, we know “our normal” and we continue to be our own best advocates. The more you know, the less intimidating the entire process is. And to top it off, when you can find a group of women like the patient advocates at the AiRS Foundation to support you along the way, you’ve got nothing to be scared of. For more information on how you can get tested for a breast cancer gene mutation, visit: beBRCAaware
By Allyn Rose