
As I write this, I’m 20 weeks pregnant. It’s unbelievable to think I’m almost halfway through my first pregnancy. Time has seemingly flown by in comparison to how long it took to get here.
I am a carrier of a rare X-linked genetic mutation that claimed the lives of three of my uncles and countless others before them. Determined to have this sad legacy end with me, my husband and I underwent the IVF process with Shady Grove Fertility, along with genetic testing on our embryos, to screen out this disease. It seems so simple typing that sentence now but it took a 10-month emotional roller coaster to get here.
As the daughter, granddaughter and niece of women who lost their lives to breast cancer, I’ve always been acutely aware of my family’s health history. Because of this strong hereditary link to breast cancer, I always feared that I, too, may suffer the same fate. Armed with that knowledge, and with the advice of my doctor, I underwent a preventive double mastectomy at 26, just 3 months shy of the age at which my mother was first diagnosed. Having lost my mother to breast cancer when I was 16 years old, I knew what it was like to face spending the rest of my life without my mother. I didn’t want my future children to ever experience that pain. So taking charge of my health in order to be alive for my future partner and future children was my main motivation. But my preventative healthcare journey didn’t end there.
Although I tested negative for a breast cancer gene mutation (which can increase your likelihood of developing breast cancer by upwards of 80%), I has tested positive as a carrier for Wiskott-Aldrich syndrome, a rare X-linked recessive disease, causing autoimmune deficiency and other potentially fatal side effects. This meant that 50% of my male children would have the disease and 50% of my female children would be carriers (like me) and be able to pass the disease on to their future children. For years, I had been counseling women in the breast cancer community with known mutations to consider IVF with PGT (preimplantation genetic testing) as a way to avoid passing on potentially deadly cancer mutations. Now it was my turn to be proactive, this time for the health of my future children.

The process involved two egg retrievals, wherein my fertility specialist, Dr. Kate Devine, prescribed me a series of ovarian stimulation drugs that I had to inject over a 2-3 week period. This caused follicles (tiny egg sacks) in my ovaries to grow and those eggs were them retrieved, fertilized, and the subsequent embryos sent to a lab for genetic testing. Again, typing it seems simple, but it involved injecting myself in the stomach several times a day for weeks in order to grow those eggs, then undergoing surgery with anesthesia to remove them and the worst part, waiting 3 weeks to hear if any of those embryos were healthy. I was devastated when my first round resulted in only one viable embryo. I knew that I wanted a big family – that meant doing it all over again (and hoping for a better outcome). I was one of the lucky ones and my second retrieval yielded 3 more embryos, leaving my husband and I with 4 mutation free potential children. We were thrilled; but the journey didn’t end there. I know had to undergo another procedure to implant the embryo in my uterus and hope that it “stuck.”
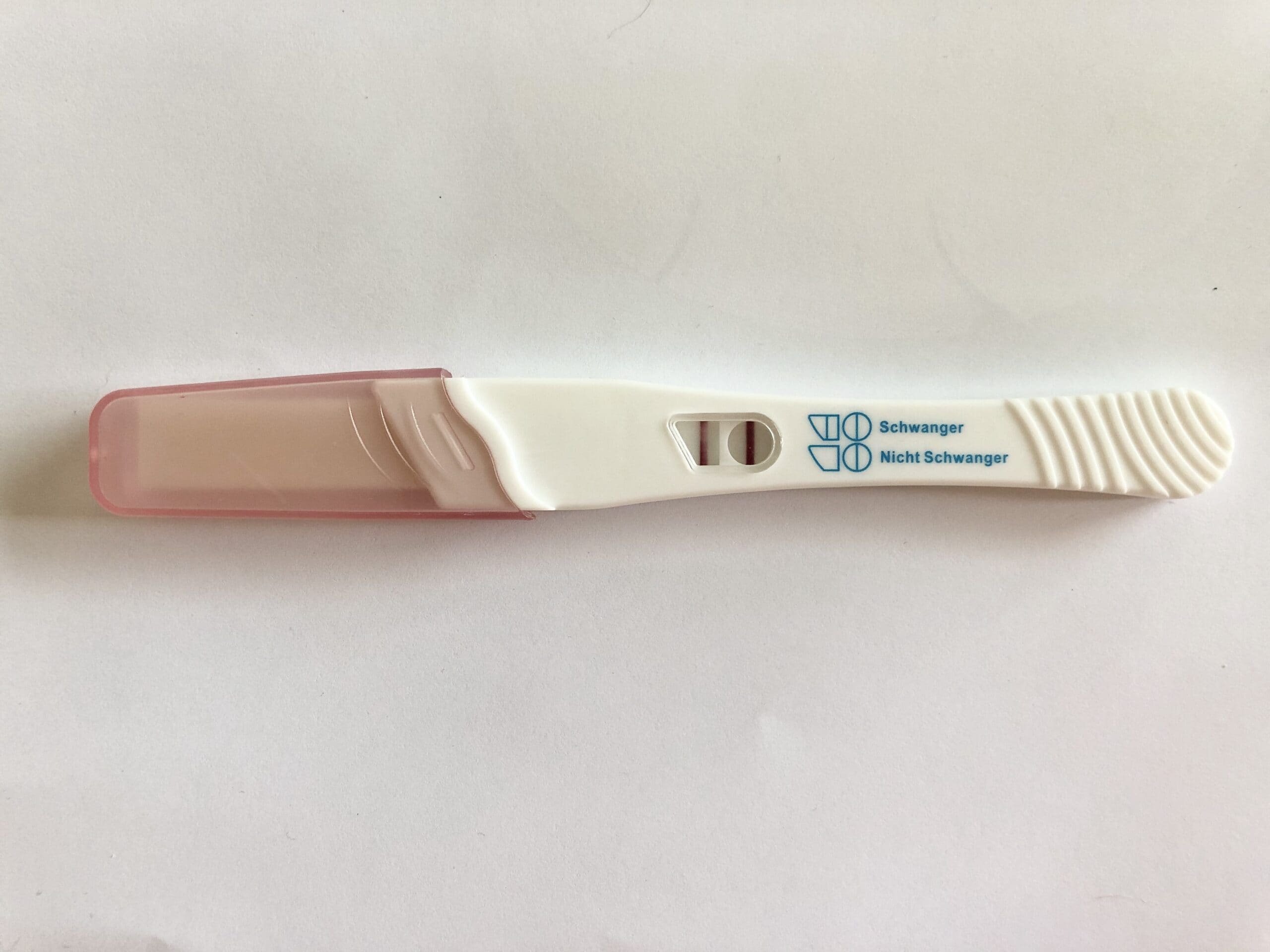
Well, 12 days after that transfer, I was greeted with 2 dark red lines on a home pregnancy test, giving me what the IVF community calls a “BFP” or BIG FAT POSITIVE!
We were part of the lucky few who got pregnant on their first try with IVF. I owe that success in large part to my wonderful team of doctors the fact that I did everything possible to ensure that the embryo implanted was as healthy as possible. I felt a sense of pride knowing that before I even met my baby, I had done everything in my power to make sure it had the best chance to succeed in life. It was my first experience “mothering.”
With another 20 weeks and a lifetime ahead of me, I truly believe that my experience with IVF helped prepare me to become a mother. It forces you to be present and deliberate in your choices, to have long term perspective and to put the needs of others before your own. I am so grateful to have had the opportunity to make positive strides towards becoming a mother, particularly during such unprecedented times (Hello, global pandemic). And although it can feel lonely at times without my own mother to guide me, I’m so thankful for the village of other women (including complete strangers on the internet) who have loved and supported my journey along the way. I couldn’t have done it without you.
By Allyn Rose

Dear Previvors,
Cancer is not going to wait for you to start your new health regimen. Cancer does not care if you just started a new job or are newly married. Cancer is not going to wait for you to have children. Cancer did not care that I was taking preventative measures and was proactively removing my breasts. It did not wait for me to find a convenient time and sadly, it’s not going to pay you a special courtesy.
I wish I had treated my positive BRCA1 test results like a cancer diagnosis. Instead, I waited too long for the ‘right’ time to take preventative measures and put myself at risk. Shortly after my 30th birthday, and just a day before my scheduled prophylactic (preventative) mastectomy, I was diagnosed with stage 3, triple negative breast cancer.
In my early twenties, I underwent genetic testing due to a significant family history of breast cancer. Testing revealed that I am a BRCA1 carrier. At that time, I was not ready for this news; I had just graduated university, was preparing to move abroad to begin my career and was not ready to think about the serious implications of this test. I promised myself then that as soon as I was secure enough in my career and had children of my own I would arrange to have a preventative surgery.
Shortly after receiving the results of genetic testing, I met with genetic counselors to discuss plans for future. I was given very high odds at developing breast cancer however preventative measures were not recommended to me at this time. Due to my age, I was unable to have mammograms and instead received annual MRI scans (a safer alternative). I thought that I was doing everything I should at the time and felt safe.
My mother was 41 years old when she was diagnosed with stage 2 breast cancer and my grandmother was 39. Due to the fact that breast cancer tends to develop earlier in later generations, as I approached the age of 30, I began to prepare myself mentally for a bilateral prophylactic mastectomy. In the fall of 2019, I met with two surgeons who would work alongside each other to remove and reconstruct my breasts. We scheduled my procedure for three months from that date and I began to prepare for this life-altering surgery.

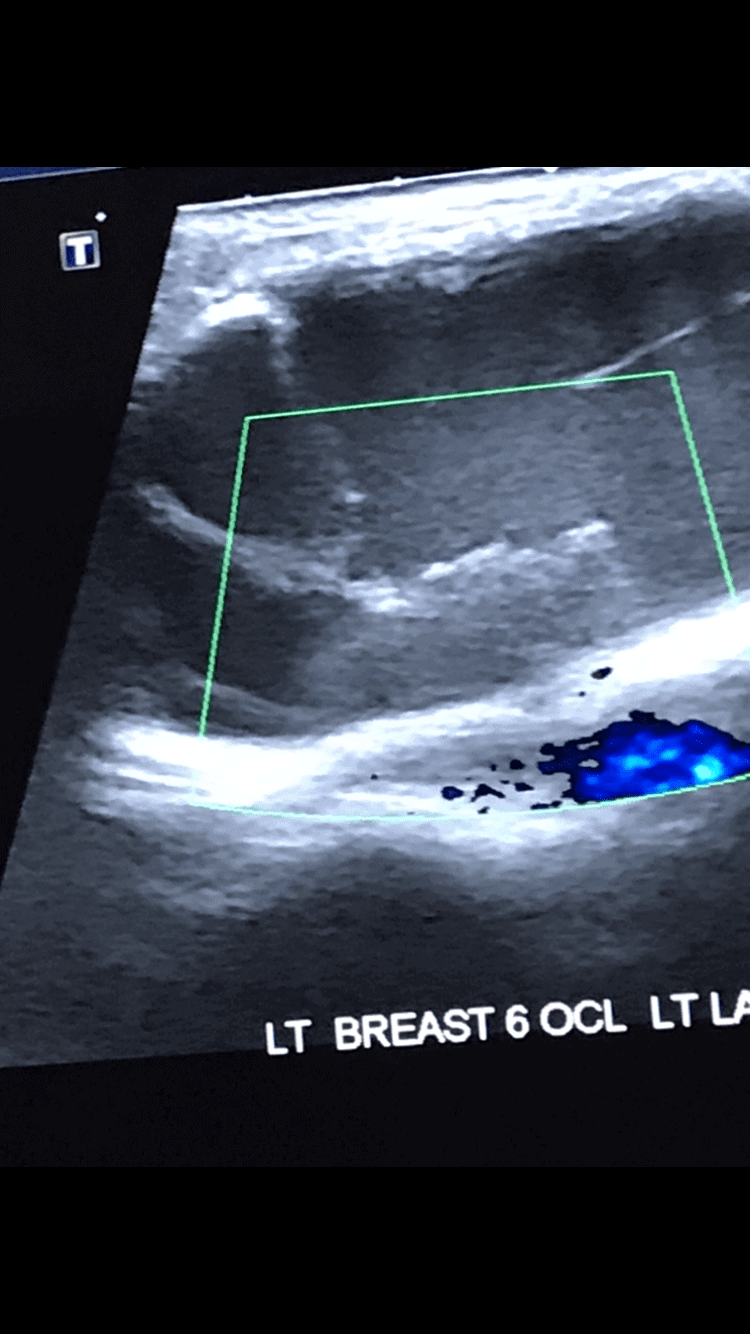
Two weeks prior to my scheduled mastectomy, I discovered a lump, the size of a golf ball, in my left breast and had to endure six excruciating biopsies. This procedure took over an hour to complete and involved a doctor chasing solid masses within a cyst in my breast. This was the most invasive, horrific experience I have had to date. Just a day before my double mastectomy my surgeon called me to inform me that the biopsy results were positive for cancer cells.
When I received my diagnose I was in absolute shock. I felt like a ticking time bomb, living in fear that I would one day develop cancer and I had worked so hard to build up the courage to have an elective surgery. It felt like a cruel joke. I cannot begin to explain the frustration and regret that I felt and continue to feel. I had years to complete this surgery and did not act.
Since my bilateral mastectomy I have not had a moment to breathe. About a week after surgery, my boyfriend and I were rushed into family planning and fertility preservation as chemotherapy can cause infertility. I struggled to walk into the fertility clinic as I was still healing. I knew little about IVF so these procedures were overwhelming to me. My boyfriend was responsible for delivering 30 injections to me, each progressively causing me more discomfort as my ovaries grew. Days following my egg retrieval, I began chemotherapy and will soon receive radiation.

Each stage of this journey has been emotionally and physically challenging.
I didn’t have time to process my cancer diagnosis as my surgery was the following day. Following my surgery, I remember all I wanted was wanting to cry and scream and let out my emotions but I couldn’t because it would physically cause my too much pain. I felt trapped inside my own body and hated myself for not taking action sooner. I went from feeling empowered and optimist about my preventative surgery to feeling like a helpless victim. I grieve the loss of my breast, loss of sensation, and the ability to breastfeed every single day. I also fear that I may no longer have the opportunity to be a mother as IVF will have its own challenges in the future. I am terrified that treatment may result in secondary cancers or that cancer will return. These uncertainties weigh heavily on me.
If you are a BRCA carrier or someone with a high risk of developing breast cancer I can confidently say that you will never be ‘ready’ and no time will ever feel ‘prefect’ to undergo preventative measures. Nothing could have prepared me for a double mastectomy and I wish I knew that sooner. Waiting could be the difference between life and death. I strong urge you to undergo preventative measures (i.e. surgery) as soon as possible. A bilateral mastectomy is stressful and challenging enough without having to undergo fertility preservation and treatment as well. Take action and control before cancer does.

If you are found to be at high risk I want you to reframe how you perceive this diagnosis. Instead of asking yourself “Why me?” or thinking “ This is not fair!”, I want you to say, “I am thankful I know now.” If you are fortunate enough to receive a warning, act on it because some women may never know they are at high risk and others worse. I am grateful to have had the opportunity to prepare for my double mastectomy. I had time to say farewell and throw a ‘boob-voyage’ with my friends’ support, I had the chance to preserve a part of myself during a boudoir session, and I had the opportunity to educate myself and take my time in finding a surgeon I trusted. Since I took action, I had more control over loosing my breasts and this had mental health benefits.
Surgery will not be easy. Being a previvor means you will be tested emotionally and physically but having control will ease the process. Being a previvor means you do not have to rush fertility or compromise it. Being a previvor means you do not have to expose yourself to toxic treatments and put yourself at risk for secondary cancers. Being a previvor means your have a network of women at your access for support both in-person and online. I strongly urge you to take action while you can still be a previvor.
By Carmela Fuca